Coping Strategies
Alongside a good treatment plan there are various things you can do to try and minimise the effects of hyperemesis gravidarum.
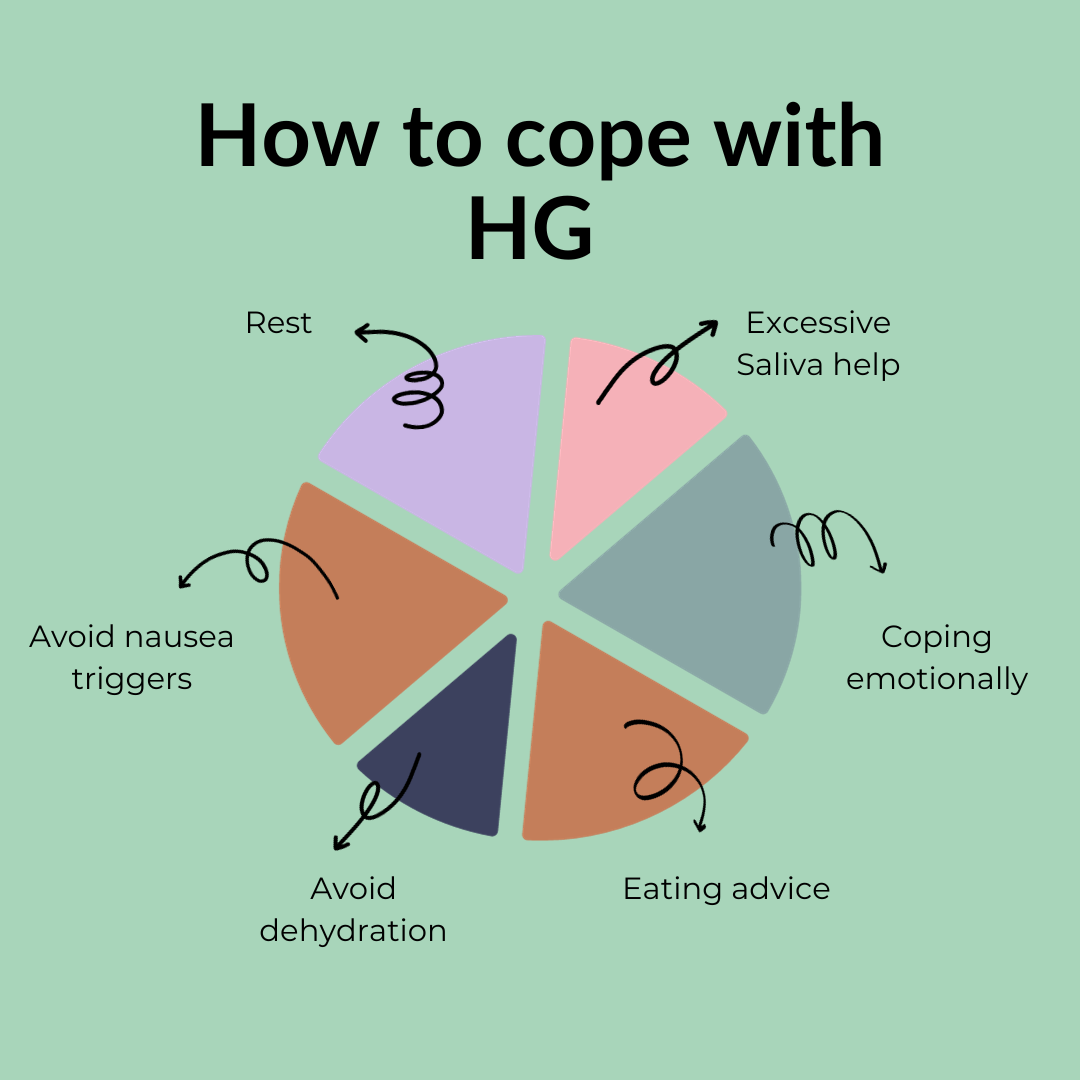
REST
The key for the hyperemesis sufferer is rest rest rest!
Don’t think you’re somehow weak because you can’t so much as do a bit of housework before having to take to your bed again, this is absolutely classic, and most HG sufferers will recognise this. If it’s your first baby, just lie on the sofa and enjoy not vomiting for a change.
If you have children, do everything in your power to sort out childcare – rely on relatives, nurseries and friends. Don’t feel guilty about needing help, you are very ill, and you would not be expected to carry on as normal if you were undergoing treatment that causes similar symptoms, such as chemotherapy.
The house may be a tip, there may be a washing mountain and the kids/your partner/work may have to fend for themselves for a while but if you push yourself, your vomiting will get worse.
If you have HG, you need to give yourself a break and know that normal service is not applicable.
COPING EMOTIONALLY
Physical and mental health go hand in hand, and it’s not unusual to suffer mentally when you’re feeling unwell for so long. If you feel you are struggling then there is help available.
- Ask your GP or midwife to refer you to the perinatal mental health team for further support.
- Contact us to be matched with a peer supporter who has been through HG themselves and can understand how debilitating this condition is. Text support from a HG survivor can be absolutely invaluable at getting you through each day and helping you feel less alone.
- Avoid thinking ahead more than the next few days. Torturing yourself with ‘I have 20 weeks of this left to go’ is not helpful. Take one day at a time and at the end of the day acknowledge that you have one less day to get through.
- Lying alone in bed or on the sofa can make you feel isolated. If you’re able to watch TV then watch your favourite films or series, or perhaps something new. If watching TV makes you nauseous, try radio or audiobooks instead. You may find music therapeutic, or adult colouring-in books, finding something which can entertain you in those moments of relief will help with the isolation and boredom.
- Having friends who can come over for a while and just be around will help a lot with the loneliness that many people feel. If you are okay to talk on the phone, call friends or family to keep you company.
- Becoming informed as possible on the treatments you can take can go a long way in feeling in control of your condition rather than having the condition control you.
EXCESSIVE SALIVA
Excess saliva (or hypersalivation) is a very common part of HG but isn’t often talked about.
It can be overwhelming and distressing to deal with, especially if you are dealing with unhelpful comments. There are some things we can suggest trying which may help, often people just need some coping tips as there is sadly very little medication available for this symptom.
- Ask your GP for an antacid called omeprazole, some people find it helpful in reducing the amount of saliva to some degree. It can also help with nausea and retching
- Carry a spit cup or cloth around with you so that you can get rid of the saliva without swallowing
- Sucking on strong flavoured sweets can help with the taste in your mouth that comes as part of HG
A complication of spitting out excess saliva can be dehydration. If you are experiencing any symptoms of dehydration, then please let your healthcare professional know as soon as possible.
HELP WITH FOOD & EATING
People with pregnancy sickness often find that the list of food and drinks that they can keep down is very small and not at all from the healthy options.
Some even find that eating vegetables and some fruits causes immediate vomiting in the peak stages, making it even more difficult to follow a healthy diet.
An empty stomach can exacerbate nausea so snacking little and often and keeping snacks nearby may help with symptoms.
It is important to follow current guidelines regarding avoiding certain foods which may contain harmful bacteria such as paté, liver, soft cheeses, and undercooked eggs, but outside of this it can just be a case of finding ‘safe’ foods that work for you.
People often find that cold, sometimes fizzy, drinks can be easier to tolerate and dry/beige foods but the list of food/drinks that work for you can be ever changing so having a variety of options to hand is helpful.
Here are some suggestions that might help with nutrition and calorie intake.
Snacks: Try to always have snacks available in the house so that as soon as you feel able to eat something you can. Snack bars or cereal bars, crisps, crackers and so on.
Fortify Meals: If you are managing to eat small amounts at your mealtimes, then try to add calories to your meal by fortifying with hard or pasteurized cheese, butter, crème fraiche, margarine, meat and so on.
Lactose Intolerance/Dairy Allergy/ Dairy Free/Vegan: Fortify your meals, snacks and drinks using pulses, (silken) tofu, avocado and dried fruits. Already fortified cereals, bread, unsweetened soya, rice, and oat drinks can be bought from the supermarket. Seeds and nut butters can also be added to meals and snacks as well as snacking on whole nuts (please avoid if allergy present). Cook and prepare any food using olive oil, coconut oil, avocado oil, or flaxseed oil.
Please don’t feel guilty if you are struggling to eat anything nutritious. If and when you feel able please speak to your GP or Midwife to see if you can be referred to a Dietician.
AVOIDING NAUSEA TRIGGERS
Understanding and avoiding triggers can be key when dealing with nausea/vomiting in pregnancy. Sensory stimuli like noises, bright lights and certain smells can be intolerable and it’s important to try and manage your environment to work around things that are challenging for you.
- Find unscented household and hygiene products.
- Brushing teeth can be hard, but using a small (children’s) toothbrush and an unscented toothpaste can help.
- Reduce exposure to cooking smells where possible.
- Bright lights can be a trigger, so try having the curtains drawn and using a lamp during the day, or even just sitting in a completely dark room if any light is too much. And remember to adjust the brightness on any screens you use regularly, like your phone or laptop.
- For smell triggers you can block out smells completely by wearing a swimming peg on your nose if you can tolerate it, or have a tissue handy with some essential oil that you can smell.
- Feeling tired or doing too much can have a big impact on how sick you feel, so make sure you’re taking regular naps and getting to bed early enough for a full 8-hour sleep.
DEHYDRATION
With HG even water can become very intolerable but try to drink an absolute minimum of 500ml a day.
Avoid dehydration by trying some of the following tips:
- Sucking ice cubes – these can be made of juice or water, whatever is more tolerable
- Sipping very slowly through a straw
- Bottled mineral water may be more palatable than tap water
- Having ice lollies
- Flat fizzy drinks can often be easier to keep down
- Seeing if you can manage foods with a higher water content such as watermelon, cucumber, oranges and grapes
If this doesn’t work and you become dehydrated, then be prepared for a hospital admission. Don’t try to fight it – if the GP says you need to be admitted you must go. Not getting treatment can lead to serious complications for you and baby. An intravenous drip and having antiemetics injected can give you days/hours of respite that are so important not only to your physical welfare but your mental wellbeing too.
Q&A with Employment Solicitor Danielle Ayres on Pregnancy Discrimination
Danielle Ayres, an Employment Partner at Primas Law, stands as a Leading Lawyer recognised in the 2023 Legal 500. With a...
Reflections on the Birth Trauma debate
This date is a moment in history: the first ever debate on Birth Trauma in the 222 year history of Parliament. And I was there....
“Suggesting ginger as a remedy for hyperemesis was damaging to my mental health.”
Rachel Brian | Scotland


