What is HG?
Please be reassured that Hyperemesis Gravidarum is not morning sickness. In fact that terminology is outdated, hence why we are called Pregnancy Sickness Support.
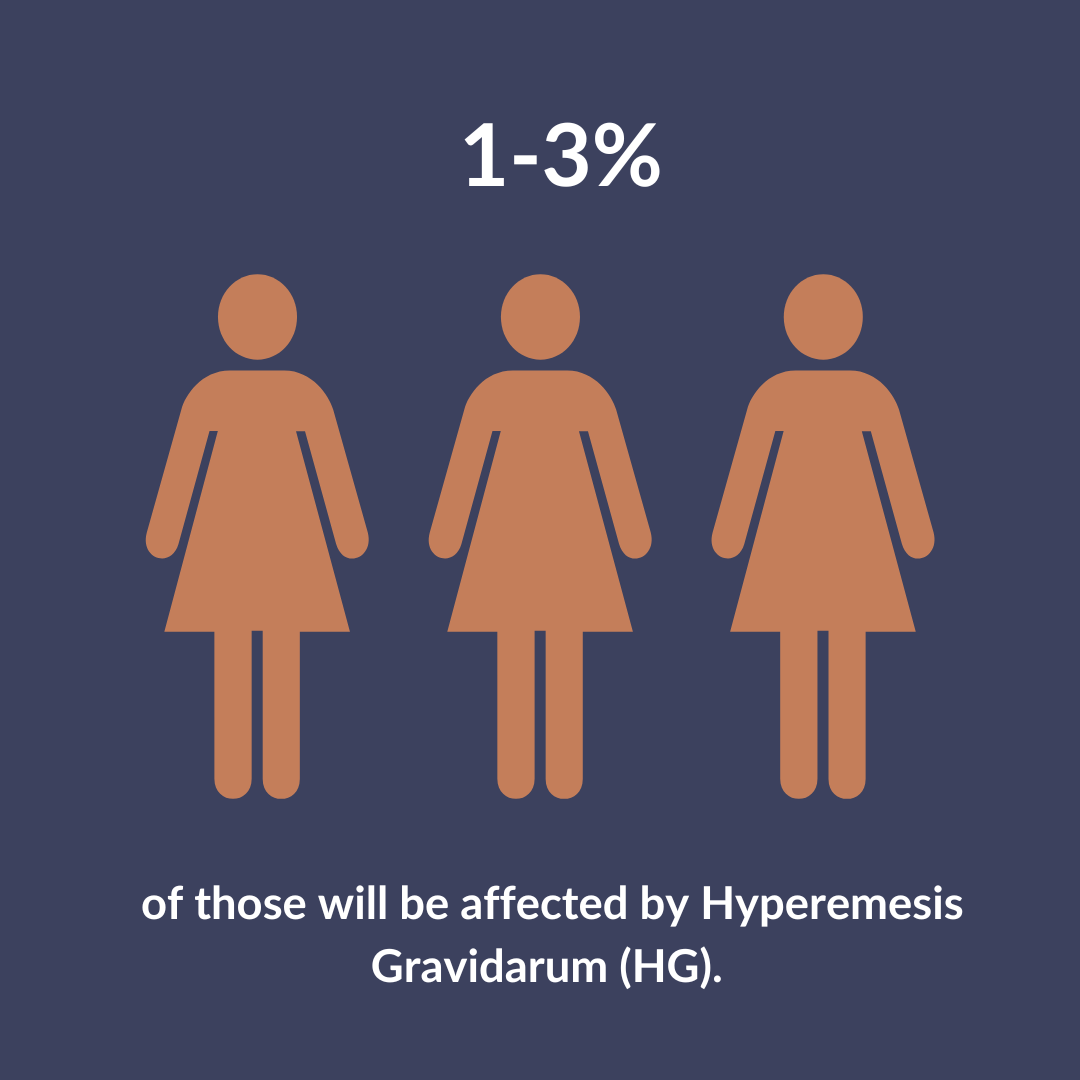
Hyperemesis gravidarum (HG) is a condition at the extreme end of the pregnancy sickness spectrum. It affects approximately 1-3% of people with pregnancy sickness and is incredibly debilitating for sufferers.
- Up to 30,000 pregnancies per year in the UK are affected by HG
- May begin very early, even before a positive test
- Symptoms peak at 9-13 weeks, can improve around 16-24 weeks but may continue throughout the whole pregnancy
- Weight loss may be severe and rapid, and dehydration is common
- If not managed appropriately complications can ensue
- Medical treatment is necessary
- Psychological support is beneficial
- Spectrum condition, not all HG looks the same
- 1 in 5 people with severe HG will have symptoms throughout their whole pregnancy.
What is pregnancy sickness?
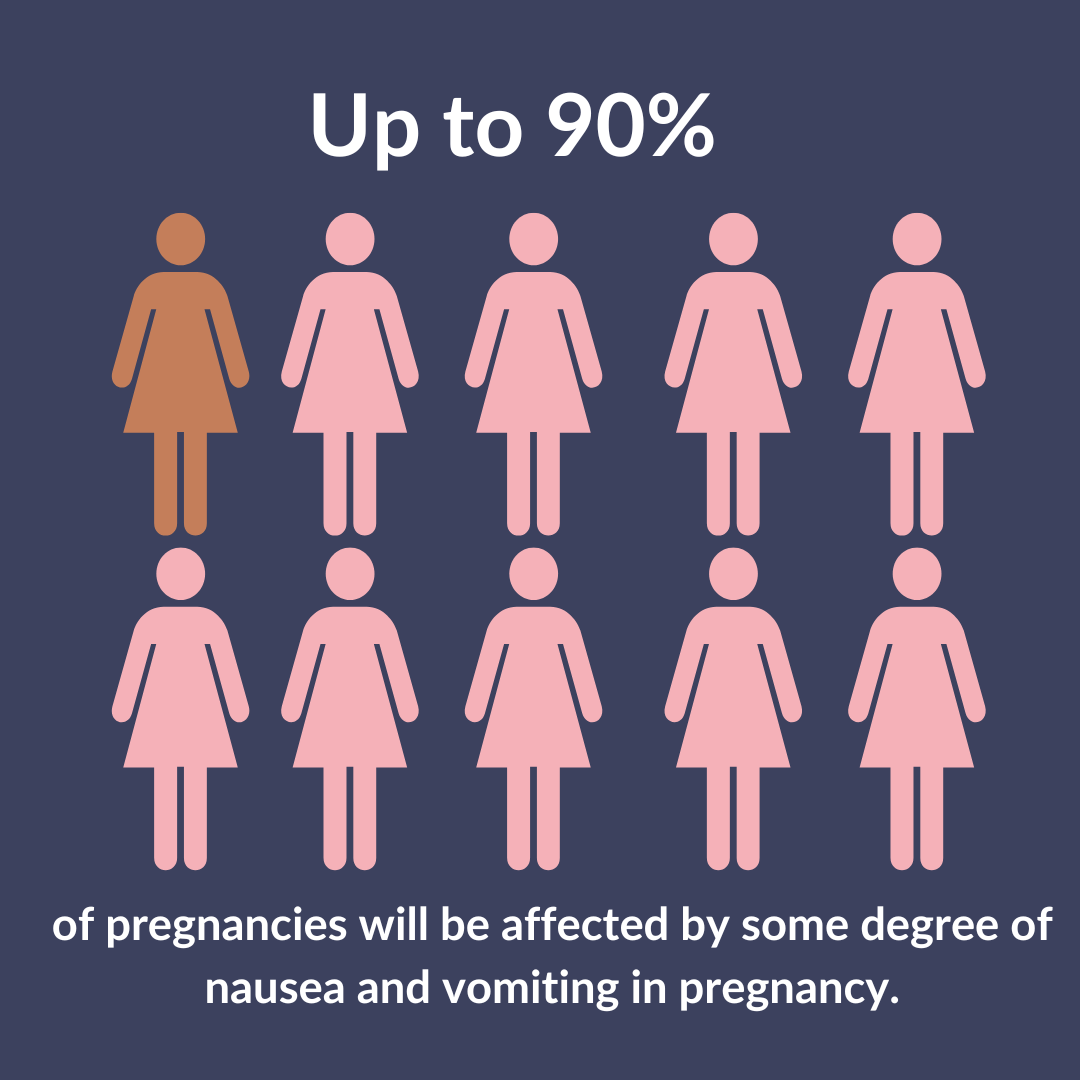
The spectrum of pregnancy sickness ranges from mild nausea and vomiting in pregnancy (NVP) to hyperemesis gravidarum (HG),with 70-90% of pregnancies affected to some degree.
Mild NVP
Often called morning sickness, though this is an outdated term as sickness can occur at any time of day, you can usually go about your normal routine without too much hinderance, and symptoms usually ease in the second trimester.
Moderate – Severe NVP
Moderate to severe NVP is often mistaken for mild NVP, which can lead to a barrier in treatment. Unlike Mild NVP sufferers will experience more persistent nausea and vomit more often.
MORE ABOUT MILD NVP
- Typically, short bouts of mild nausea and/or occasional vomiting
- Generally, no negative physical or mental impact
- Usually lasts for the first trimester
- Can be managed through diet and lifestyle changes
- An often expected and wanted experience.
MORE ABOUT MODERATE - SEVERE NVP
- Some people experience excessive saliva
- Can last to 20 weeks and beyond
- Diet and lifestyle alterations may help but medication is most likely appropriate
- Emotional and psychological support may be needed
- Quality of life impacted
- May lose weight.
WHAT IS HYPEREMESIS GRAVIDARUM?
As detailed above, hyperemesis gravidarum (HG)is a condition at the extreme end of the pregnancy sickness spectrum. It affects approximately 3% of pregnancies and is very debilitating for sufferers. HG strongly limits everyday activities; vomiting and/or nausea are severe.
It is important that you seek medical treatment if you are unable to keep any food or fluid down as you can become dehydrated very quickly. Often IV fluids are essential to become rehydrated, and medication is necessary to try and stabilise symptoms. Contact us to talk through your options and to help you advocate for yourself with your healthcare professionals.
When do I seek help?
Now. Chances are you are reading this page because you have sickness in pregnancy and are not sure if what you are going through is ‘normal’. Especially in a first pregnancy, or first pregnancy with sickness, it can be hard to know when to seek help.
As soon as the quality of your life is impacted, and you can’t go about your usual routine then it’s time to seek medical support. Before contacting your GP or midwife chat with our support team so you can prepare yourself with all the correct and up to date information. Early treatment could reduce admission rates to hospital and prevent dehydration so seek support as soon as you can after your symptoms start. Some GPs can refer you to a consultant if your symptoms are particularly bad, or if you have previously had a severe HG pregnancy, then consultant care may be beneficial from early on in a subsequent pregnancy.
You can read more about treatment here
WHAT HAPPENS NEXT?
If you are experiencing clinical signs of dehydration, IV fluids and medication are needed.
- Visit your local Early Pregnancy Unit or A+E; hospitals have different admission protocols.
- Contact the support team for assistance regarding local options.
- Communicate symptoms precisely to healthcare professionals for appropriate treatment.
- Important details to share include:
- Frequency of vomiting per day.
- Duration of nausea in hours.
- Frequency of retching per day.
- Daily intake of liquids (in millilitres) and ability to keep them down.
- Daily intake of food (in bites or portions) and ability to keep it down.
- Changes in urine, such as darker color, reduced frequency, or decreased amount.
- Other dehydration symptoms: dry mouth, dry lips, headaches, dizziness, weakness, confusion, and disorientation.
How do they assess the severity of pregnancy sickness?
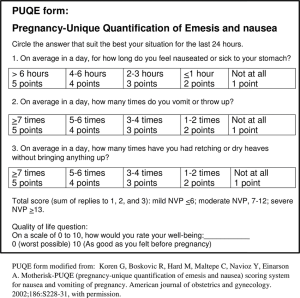
The Pregnancy-Unique Quantification of Emesis (or PUQE score for short) is an assessment tool which healthcare professionals could use to help them to determine the severity of your symptoms and where you may be sitting on the pregnancy sickness spectrum. Each question has a score between 1 – 5 depending on your answer, and the total number scored can be used to get a better understanding of where you may be on the pregnancy sickness spectrum.
There are other things that you should take into consideration also:
- Are your symptoms affecting your ability to eat and drink?
- Have you lost weight since you became pregnant? If so how much?
- Are your symptoms making it hard to function normally?
- Are you having to take time off from work?
- Are you struggling to do day to day normal activities or even just to get out of bed?
If you answer yes to one or more of these questions, then you need to seek medical support.
THE PUQE SCORE
“The baby growing in the womb is producing a hormone at levels the mother is not used to. The more sensitive she is to this hormone, the sicker she will become.“
Professor Stephen O’Rahilly | University of Cambridge
